New Bill Would Allow Legal Heroin Use In ‘Safe Injection Sites’
This article originally appeared on Kaiser Health News.
Tawny Biggs’ seemingly happy childhood in the northern Los Angeles County suburb of Santa Clarita, Calif., showed no outward sign that she would one day struggle with drug addiction.
As Biggs tells it, she was raised with two siblings “in a very good family” by an assistant fire-chief dad and a stay-at-home mom. Her after-school hours were filled with hockey and soccer.
But paradise was lost sometime during her late teens, when emotional problems, drugs and alcohol turned Biggs into a self-described “nightmare.” One night, when she was amped up on cocaine, her boyfriend gave her a hit of something different to help her sleep: heroin.
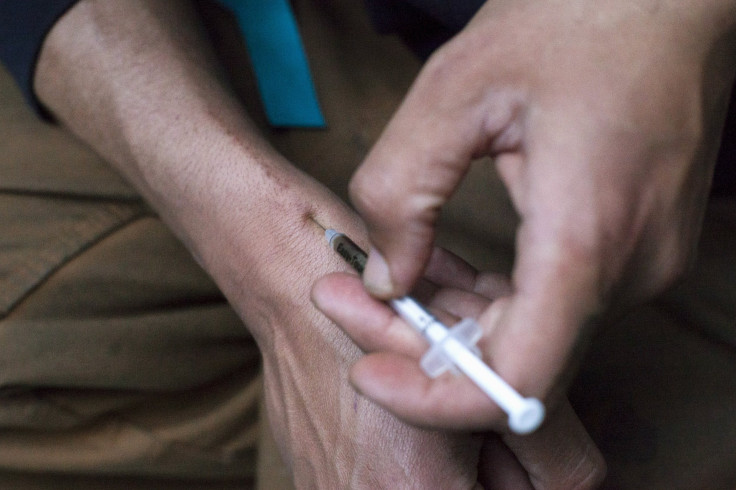
Before she even knew what had happened, she was addicted. Six months later, she learned she had contracted hepatitis C from a dirty needle.
Biggs, now 37, finally got sober 14 years ago. Now, she helps others get clean as an admissions coordinator at Action Family Counseling drug and alcohol treatment centers, in her hometown. Based in part on her own arduous experience, she strongly supports a controversial proposal to establish venues where adult intravenous drug users can shoot up with clean needles under medical supervision and get referrals to addiction treatment.
The only injection facility currently operating in North America is in Vancouver, Canada. Australia and several countries in Europe also have such centers.
“I think it’s a great idea,” said Biggs. “Right now, in this climate, we have to think out of the box because we’re fighting an uphill battle.”
A bill pending in the state legislature, AB 186, would authorize eight California counties — Alameda, Fresno, Humboldt, Los Angeles, Mendocino, San Francisco, San Joaquin and Santa Cruz — to test so-called “safe injection sites.”
The legislation faces tough opposition. Critics say it essentially endorses the use of illicit drugs. And it is not likely to sit well with the federal government, particularly under Attorney General Jeff Sessions, whose hard line on drugs is well-known.
Advocates argue, however, that a different approach is needed to stem the rising tide of addiction and related deaths.
Earlier this spring, San Francisco’s Board of Supervisors instructed the Department of Public Health to form a task force to make recommendations on the establishment of safe injection venues.
Nationwide, several major cities — including Seattle, Baltimore and Philadelphia — are considering such publicly sanctioned locations as a means to curb escalating heroin drug overdoses and deaths; slow the spread of infectious diseases such as hepatitis C; and help people kick their lethal habits.
Across the United States, an exploding opioid epidemic has sent overdose deaths skyrocketing and policymakers scrambling for solutions. In 2015, opioid overdoses — both from prescription drugs and from more potent and easier-to-obtain street heroin — took the lives of 2,018 Californians and 33,091 Americans, according to data from the Kaiser Family Foundation. (California Healthline is produced by Kaiser Health News, an editorially independent service of the foundation.)
“This is a medical issue, it is a brain disease, and we have to get out of our shell of thinking that these are bad people and … they have to hit bottom and then decide to pull themselves up by their own bootstraps,” said Barbara A. Garcia, director of health at the public health department in San Francisco, where 22,000 residents are known IV drug users. “That’s the pathway to death.”
Safe injection sites would go beyond existing needle exchanges by allowing drug use on the premises. Under the proposed California measure, introduced by Assemblywoman Susan Talamantes Eggman (D-Stockton), health care providers stationed at the sites would be armed with the emergency medication naloxone, which is used to help revive people from opioid overdoses.
“What we’re talking about here is essentially a medical facility,” said Christian Burkin, a spokesman for Eggman. “This is an opportunity to take drug abuse off the streets and put it into a safe and sterile environment.”
Opponents of the measure, including many law enforcement organizations, fear such sites would only serve to normalize illicit drug use and harm local neighborhoods.
“It creates a danger for the communities that these safe consumption program sites would be located in,” said Cory Salzillo, legislative director for the California State Sheriffs’ Association. “It doesn’t require anybody to undergo treatment. … It’s just effectively: ‘Here’s a safe place for you where you can come; here’s your needle, your paraphernalia and here you go, shoot up.’”
Even if the state measure were to pass, it might face significant resistance from the federal government, since the drugs that would be injected are illegal under U.S. law, said Stanley Goldman, a criminal law professor at Loyola Law School in Los Angeles.
“So you’d have to be fairly assured that the federal government was not going to proceed against such operations before people could feel completely comfortable with participating,” Goldman said.
Cary Quashen, president and founder of the Santa Clarita rehabilitation center where Biggs works, said that while he also has some reservations, he’d be likely to support the concept as long as drug users are offered access to recovery services at the centers.
“We got to do something different. People are dying everywhere,” Quashen said. “We lose more people in this country to accidental overdoses than to car crashes and gun violence.”
Burkin noted that the proposed safe injection clinics would be restricted to areas “where they are experiencing a high rate of opioid abuse, including death.”
A 2011 study published in The Lancet found that overdose deaths on the streets surrounding Vancouver’s safe injection site dropped 35 percent in the two years after it opened, compared with the two prior years. In the rest of the city, overdose deaths dropped 9.3 percent during the same period.
Another study showed a 30 percent increase in the use of addiction treatment services associated with the opening of the Vancouver site. Studies also suggestthat supervised injection facilities in Australia and Europe have reduced overdoses without an increase of drug injecting or trafficking in their communities.
“We are not supporting what people call ‘shooting galleries,’” said Garcia, the San Francisco public health director. “I don’t believe in allowing people to just sit in a room and shoot drugs with each other — that is not something I’m going to support. What I will support is how do we engage those who are using drugs to help them reduce their harm and get better and go into recovery eventually.”
Another argument in favor of supervised injection sites is financial: Two recent studies showed that a single supervised injection site would save $3.5 million a year on health care costs in San Francisco and $6 million in Baltimore.
Burkin believes that, given a chance, the safe injection pilot programs will prove their worth.
“Someone addicted to opioids who is going to come to a facility like this is someone starting on the first step toward recovery,” he said. “This is not someone who is going to ignore appeals or attempts to get them connected to services.”
Tawny Biggs agrees. If it were not for a work colleague in recovery who introduced her to a 12-step program years ago, she said, she would not have survived.
When her boyfriend gave her that first hit of heroin, she said, it didn’t seem like a big deal.
“I was thinking, ‘I can handle this,’” Biggs recalled. “Then something snapped in my brain and there became no control over needing it. I knew at that point it was either I gave up my son to my mom and shot up dope until I died, or I got some sort of help.”
This story was produced by Kaiser Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.





















